On Monday, August 30, 2021, the Advisory Committee on Immunization Practices (ACIP) voted unanimously to approve a recommendation that stated:
The Pfizer-BioNTech Covid-19 vaccine is recommended for people 16 years of age and older under FDA’s Biologics License Application (BLA) approval
This recommendation was quickly endorsed by CDC Director, Dr. Rochelle Walensky.
- In approving this recommendation, ACIP heard evidence from Pfizer, Kaiser Permanente, CDC, and other scientists on the safety and effectiveness of the vaccine.
- Apparently fully or partially absent from this evidence were six studies, cited in a post-vote presentation. These studies, including those by CDC and Pfizer scientists, describe waning vaccine effectiveness, or effectiveness against the delta strain, from the 90-95% range to, in one case to as low as 42%.
- The inclusion of these missing studies would have yielded a different risk-benefit analysis.
- Given the ramifications this recommendation is already having on vaccine mandate policy, the evidence presented to ACIP does not appear to meet the highest level of standards for scientific integrity and conduct.
- Other intense safety signals, such as a 177 times increase in the number of deaths per vaccinated person reported for Covid-19 vaccines, compared with flu vaccines, were not considered.
- ACIP did not consider the possible effects of the vaccines on pregnancy or the reproductive system, hinted at by the announcement the same day by NIH, to fund studies on the links between the Covid-19 vaccines and menstrual disorders.
- ACIP did not consider other possible long-term effects (cancer, autoimmune disease) of the vaccines related to their falling under the FDA classification of a “gene therapy product,” and made no comment about the lack of studies performed by Pfizer/BioNTech “for the potential to cause carcinogenicity, genotoxicity, or impairment of male fertility.”
- The significant short and potentially long-term cardiac, vascular, hematological, musculoskeletal, intestinal, respiratory or neurologic symptoms health issues stemming from the use of these vaccines pose a major and expensive public health problem.To concretize recognition of, and to spur action to avert and confront this potential public health crisis, we have proposed the term:
Post Covid Vaccine Syndrome – pCoVS
- There needs to be:
- Assignment of ICD10 and related tracking or reimbursement codes for pCoVS.
- Funding for research and tracking for long-term and delayed pCoVS.
- Regulation of the Pfizer, Moderna, and Janssen vaccines as Gene Therapy products, requiring long-term follow-up.
- Since FDA and CDC cannot assure us about the safety of two vaccine doses, how can they give any assurance about a third (or more doses)?
Introduction
On Monday, August 30, 2021, the Advisory Committee on Immunization Practices (ACIP) voted unanimously to approve a recommendation that stated:
The Pfizer-BioNTech Covid-19 vaccine is recommended for people 16 years of age and older under FDA’s Biologics License Application (BLA) approval
Shortly thereafter, Dr. Rochelle Walensky, Director of the Centers for Disease Control and Prevention (CDC), endorsed this recommendation,[1] adding
“We now have a fully approved COVID-19 vaccine and ACIP has added its recommendation. If you have been waiting for this approval before getting the vaccine, now is the time to get vaccinated and join the more than 173 million Americans who are already fully vaccinated,”
Once the recommendation is published in CDC’s Morbidity and Mortality Weekly Report (MMWR), this statement will “represent the official CDC recommendations for immunizations in the United States.”[2]
Within the fine print of the evidence presented to ACIP prior to its vote, are details that suggest that the vote may have been influenced by possible scientific misconduct.
What happened? Who was voting and why?
Unlike FDA, whose mission is to ensure that medical products can only be marketed if they are safe and effective, CDC[3] “conducts critical science and provides health information that protects our nation…” Advising the CDC are specialist and expert committees such as the Advisory Committee on Immunization Practices (ACIP) composed of non-government scientists, doctors, health professionals, and community representatives.
ACIP was asked by CDC to formulate a recommendation regarding the use of the Pfizer-BioNTech vaccine. To inform ACIP’s decision, scientists and doctors from Pfizer BioNTech and CDC provided evidence concerning the vaccine’s safety and effectiveness as well as a risk-benefit analysis.
I along with colleagues, submitted pre- and post-meeting comments,(1,2) some of which are included in this article.
How safe is the Pfizer-BioNTech vaccine?
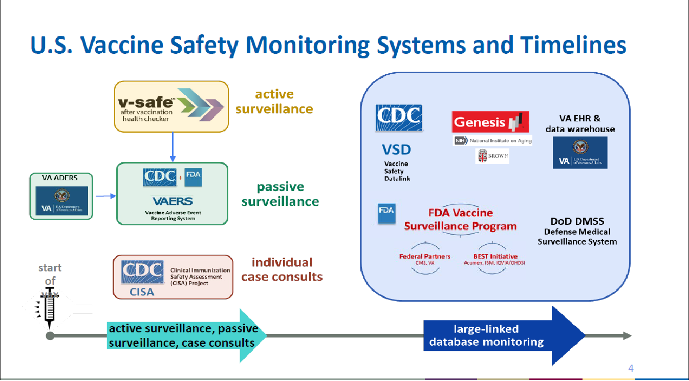
The safety discussion drew from several of the systems used to monitor vaccine safety shown on slide 4 from the presentation of Dr. Grace Lee, the chairperson of ACIP.
Focus on myocarditis
The safety discussion focused on myocarditis (inflammation of the heart muscle), particularly in younger subjects. One CDC presentation[4] cited a study published in NEJM (3) reporting a 3 times higher risk of myocarditis associated with Pfizer-BioNTech vaccination, compared with an 18 times higher risk associated with SARS-CoV-2 infection. In other words, a 18/3 = 6 times greater risk of myocarditis if you get Covid-19 than if you have the vaccine. This figure of 6 agreed with a non-peer-reviewed preprint study looking at mRNA vaccines(4) (two other CDC studies showing higher numbers were cited, but these studies have not been published – remember that – and only available to CDC internally). This is a six-fold increase IF contracting Covid. What the presentation did not say is that this is canceled out by the (at best) 1 in 8 chance of getting Covid-19 in the first place!
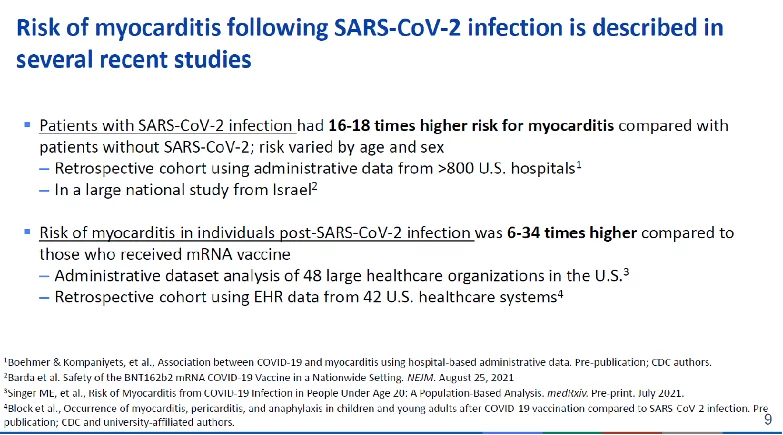
Slide 9 from presentation by Dr. Rosenblum (footnote 4)
Deaths and myocardial infarctions missing from safety discussion
What else was not mentioned? In written comments my colleagues and I (1) submitted to ACIP prior to the meeting, we compared the number of reports in VAERS for either death or myocardial infarction (heart attack) associated with the Covid-19 and flu vaccines. Adjusting for the number of doses given. There were 91 times more deaths and 126 times more heart attacks for the Covid-19 vaccines compared with the flu vaccines. If adjusted by the number of people receiving at least one dose, the figure for deaths is about 177 (July 30 figures).
This does not PROVE that the vaccines were the cause of these events. But that’s not the point. This is called a signal. It is a very intense one and awaits a transparent explanation[5] that includes a comprehensive report of the types and numbers of investigations performed, including autopsies. Although CDC has provided guidance for the conduct of autopsies of Covid-19 cases, there is no prospective protocol for the conduct of autopsies to determine whether or not the death is vaccine-related. This would include a detailed description of the types of histopathological methods to distinguish vaccine-induced spike protein from spike protein derived from a Covid-19 infection. Where is this analysis? Where is there a protocol? Similarly, the strong signal of heart attacks in younger than in older people (403 vs. 88, Table 1) must be investigated.
In our submitted comments,(1) we identified three separate pools of vaccine-associated deaths, totaling 45,000-147,000 deaths that should be viewed in the context of the upper estimate of 140,000 lives saved due to the vaccines (to May 2021).(5)
- Non Covid-19 deaths under-reported in VAERS – 20,400-62,500
- Covid-19 deaths in vaccinated subjects – 25,000-85,000
- An unknown number of deaths in non-vaccinated contributed by transmission from vaccinated people.
It is important to distinguish between these three pools, as each may have separate sets of causes. In the first pool early, non-Covid-related deaths may be related to the toxicity of the spike protein towards heart cells and effects on coagulation. Covid-related deaths may have resulted from post-vaccination immune suppression, possibly hinted at by a 40% -vaccine-associated increase in Herpes zoster infections reported in a large Israeli study(3) and referenced in one of the CDC presentations to ACIP.[6] Covid-19 may have been unwittingly transmitted by vaccinees to the non-vaccinated(6,7), including by fecal aerosol(8) in subjects sharing bathrooms.
The Precautionary Principle places the burden of proof on CDC to convincingly rule out an association between these events and the Covid-19 vaccines.
Table 1: Signals of deaths or myocardial infarctions reported in VAERS for COVID-19 vaccines compared with Flu Vaccines
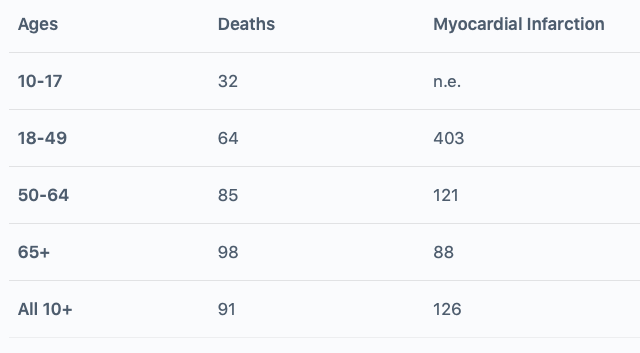
The number shown is the ratio of the number of VAERS reports (per dose) for the Covid-19 vaccines in comparison with the Flu vaccines (2015/16-2019/20 flu seasons) for each age group. Covid-19 reporting rates include all reports to VAERS for COVID-19 vaccines as of Aug. 6, 2021. n.e not estimable. Excerpted from (1).
Critics of these sorts of analyses have claimed there may have been overreporting related to enhanced reporting requirements pursuant to Emergency Use Authorization.[7] A number of the CDC presentations referenced data from VAERS without expressing any such concern. Indeed, the point was made in one presentation, that for myocarditis/ pericarditis at least, the VAERS and VSD (Vaccine Safety Datalink[8]) incidence data, agreed closely.
This similarity was not sufficient to generate a safety signal (age unstratified) for myocarditis[9] within the VSD system which uses a signal detection method called Rapid Cycle Analysis (RCA). Although in theory, RCA should be able to detect signals in near real-time as medical records are being generated in a system such as Kaiser Permanente, the method appears even less sensitive than the methods prescribed for VAERS(9) which themselves have known limitations.(1) From VAERS, myocarditis is acknowledged to be an issue as a warning in the COMIRNATY package insert attests: (10)
“Postmarketing data demonstrate increased risks of myocarditis and pericarditis, particularly within 7 days following the second dose.”
A paper was published in JAMA (11) on September 3rd describing the findings from the Rapid Cycle Analysis of the VSD system. It concluded that:
“incidence of selected serious outcomes was not significantly higher 1 to 21 days postvaccination compared with 22 to 42 days postvaccination.”
I suggest that publication of this paper without the context of the acknowledged myocarditis signals from VAERS, within the conclusion, is highly misleading.
Long term harms missing from safety discussion: gene therapy products, cancer
Also missing from the discussion were potential long-term effects of these vaccines, given that they also meet FDA’s definition for Gene Therapy products. .(12) Indeed, in 2020 Moderna acknowledged(13) that ”Currently, mRNA is considered a gene therapy product by the FDA.” Why is this important? Because FDA, is (appropriately) concerned for the effects of the gene therapy product on malignant (cancer), neurologic, autoimmune, hematologic, or other disorders. The concern is so great that FDA may require follow-up evaluations of study patients for between 5 and 15 years. When did FDA decide to ignore its own guidance document? (12) [10]
The package insert(10) for the vaccine that was approved by the FDA on August 23rd states that “COMIRNATY has not been evaluated for the potential to cause carcinogenicity, genotoxicity, or impairment of male fertility.” Neither in the BLA Approval letter,(14) nor in the Summary Basis for Regulatory Approval(15) is there a POST MARKETING REQUIREMENT to conduct studies on carcinogenicity, genotoxicity, or male fertility.
Effects on reproductive system missing from safety discussion: menstrual disorders
What else was missing? On the very same day, CDC staff were providing evidence to ACIP on the safety of the Pfizer vaccine, NIH made the startling announcement[11] that it was funding studies “to explore potential links between COVID-19 vaccination and menstrual changes.” They elaborated: “Some women have reported experiencing irregular or missing menstrual periods, bleeding that is heavier than usual, and other menstrual changes after receiving COVID-19 vaccines.” Was CDC not aware of this?
But the operative word here is “Some.” A query in VAERS (9/3/21) for various menstrual disorders[12] revealed that for reports associated with the Covid-19 vaccines, “some” means.
7037 separate menstrual disorder-related symptoms were described in 4783 unique reports.
Some? By comparison with all other vaccines, for ALL years COMBINED we have 897 symptoms in 798 unique events. Most of these are accounted for by the HPV vaccines (698 symptoms in 623 events) with seasonal flu vaccines contributing only 47 symptoms within 45 unique events.
Having worked extensively in the area of women’s health for most of my career,[13] I reluctantly confess that this was not on my radar screen. Concerns had been raised from animal studies showing the distribution of some vaccine components to the ovaries. Some menstrual effects were picked up in another analysis.(16) However, I know that “menstrual disorders” are far too often trivialized. A number of these disorders lead to early hysterectomies triggering further complications including adhesions, pain, bowel obstruction, heart disease, and dementia. Will these sorts of problems be considered in risk-benefit analyses?
NIH illustrates a number of reasons for these reported menstrual changes. No doubt out of an intense desire to be transparent with the American public in disclosing ALL of the possible reasons for these menstrual changes, NIH included in their list “pandemic-related stress.” But stress is not our prime suspect. Effects on the ovaries and uterus are, and we must view these reported menstrual changes in the context of unresolved questions about the safety of the vaccines on the reproductive system in general, and on pregnancy in particular.
Preliminary findings of a CDC study(17) published in June involving 35,691 pregnant v-safe surveillance system participants and 3958 participants enrolled in the v-safe pregnancy registry (only 827 of whom had a completed pregnancy), “did not show obvious safety signals among pregnant persons who received mRNA Covid-19 vaccines.” The study acknowledged that “more longitudinal follow-up, including follow-up of large numbers of women vaccinated earlier in pregnancy, is necessary to inform maternal, pregnancy, and infant outcomes.”
The results of a follow-up report from this CDC study,(17) appeared in NEJM on September 8th (18), and were surely known at the time of the ACIP meeting. With the startling absence of a randomized control group, the report concluded that:
“our findings suggest that the risk of spontaneous abortion after mRNA Covid-19 vaccination either before conception or during pregnancy is consistent with the expected risk of spontaneous abortion; these findings add to the accumulating evidence about the safety of mRNA Covid-19 vaccination in pregnancy”
In my opinion, this conclusion overreaches to the point of recklessness as it conflicts with and downplays the guidance provided in the COMIRNATY package insert(10) under a subheading “Risk Summary”:
“Available data on COMIRNATY administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.”
Not that the package insert, overall is much better at providing clear guidance for pregnancy. It states: “There is a pregnancy exposure registry for COMIRNATY. Encourage individuals exposed to COMIRNATY around the time of conception or during pregnancy to register by visiting this.”
As stated in their approval letter,(14) the best the FDA has done to determine what sorts of risks are posed during pregnancy is to obtain the commitment from BioNTech to conduct a post-marketing pregnancy/neonatal study with a four-year term.
Study C4591022, entitled “Pfizer-BioNTech COVID-19 Vaccine Exposure during Pregnancy: A Non-Interventional Post-Approval Safety Study of Pregnancy and Infant Outcomes in the Organization of Teratology Information Specialists (OTIS)/MotherToBaby Pregnancy Registry.”
Note the word commitment. As FDA explains[14]
“Postmarketing commitments (PMCs) are studies or clinical trials that a sponsor has agreed to conduct, but that are not required by a statute or regulation.”
This is not a requirement (as for some of the other post-marketing studies on myocarditis for example). Compare not only this level of regulation but also the length and scope of the study in question with an unrelated Janssen (J&J) biologic product for which a 7-year[15] study is required and which includes examining effects on child and early development. A recently approved (2021) Astra-Zeneca biologic product[16] requires a NINE-year study on pregnancy and maternal and fetal/neonatal outcomes.
Inadequate risk-benefit analysis
None of this featured in the evidence CDC gave to ACIP. Indeed, the only harm of any note in the risk-benefit analysis (itself focusing on 16–29-year-olds) was myocarditis.[17]
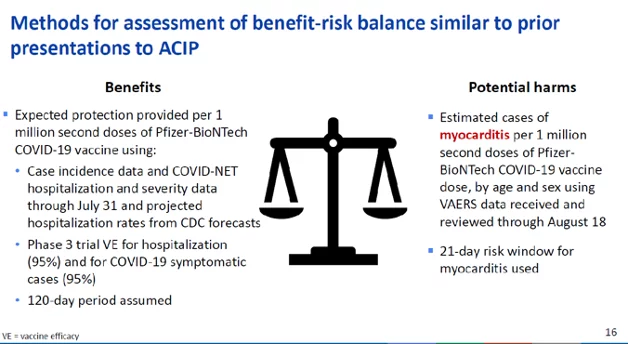
Slide 16 from presentation by Dr. Rosenblum (footnote 4)
Post-Covid Vaccine Syndrome
The sheer number of deaths or other events reported in VAERS for the Covid-19 vaccines (similar to all deaths or events reported for all other vaccines in all years combined) cannot be ignored. The significant short and potentially long-term health issues stemming from the use of these vaccines pose a major and expensive public health problem.To concretize recognition of, and to spur action to avert and confront this potential public health crisis, we have proposed the term:
Post Covid Vaccine Syndrome – pCoVS
defined as:
A syndrome occurring after injection of antigen-inducing, gene therapy vaccines to SARS-Cov-2 virus. The syndrome is currently understood to manifest variously as cardiac, vascular, hematological, musculoskeletal, intestinal, respiratory or neurologic symptoms of unknown long-term significance, in addition to effects on gestation. Manifestations of the syndrome may be mediated by the spike protein antigen induced by the delivered nucleic acids, the nucleic acids themselves, or vaccine adjuvants. As more data become available, subsets and longer-term consequences of pCoVS may become apparent, requiring revision of this definition.
We(1) have proposed:
- Recognition by public health agencies, governments, and professional societies of pCoVS.
- Assignment of ICD10 and related tracking or reimbursement codes for pCoVS.
- Establishment of transparent systems to monitor and track for long-term and delayed pCoVS.
- Establishment of funding for research into the prevention and treatment of pCoVS.
- Regulation of the Pfizer, Moderna, and Janssen vaccines as Gene Therapy products.
- Insistence on long-term (15 years) pharmacovigilance by manufacturers of these vaccines for pCoVS consistent with FDA guidelines for gene therapy products.
- Legislation to prevent discrimination based on vaccination[18] or actual or potential pCoVS status.
- Establishment of funding to determine what effects the gene therapy vaccines have on the genome or gene expression.
How effective is the Pfizer BioNTech Vaccine
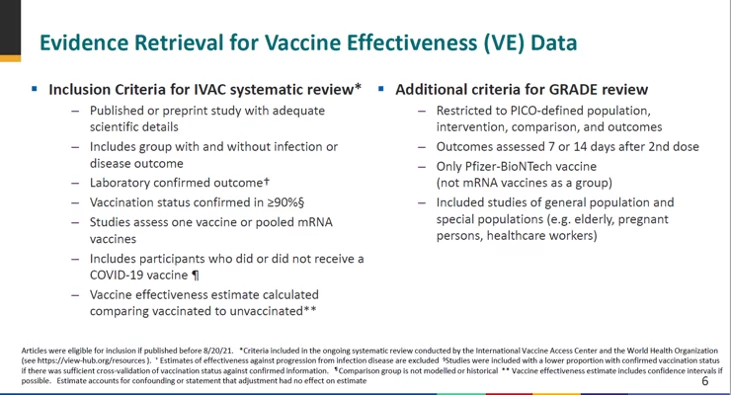
Inclusion of outdated, non-RCT, observational and non-peer-reviewed studies
Contributing significantly to the analysis by several presenters of safety and efficacy, as well as the risk-benefit analysis for the Pfizer vaccine was Pfizer’s own RCT of about 40,000 subjects[19] which was recently released as a non-peer-reviewed pre-print.(19) It was widely recognized throughout the discussion that these data only reported safety and effectiveness data for up to six months of the Pfizer vaccine, for data collected up to March 13 2021. Does Pfizer have data collected after March 13?
The use of observational or non-peer-reviewed (preprinted) studies by proponents of re-purposed drugs has been heavily criticized by public health officials as well as the media, who have insisted on evidence from large peer-reviewed RCTs. It was with some wonder that observational and non-peer-reviewed studies were included in one of the key analyses (slide 19)[20] provided to support ACIP’s recommendation, 17 observational studies, including 7 non-peer-reviewed, were employed. During the discussion, the presenter (Dr. Gargano) concurred with one of the discussants that there was good agreement between data from observational and RCT sources. Only one RCT was included19 with reference to additional about-to-be published (NEJM) study (remember that).[21]
Of these 17 studies, one reported data with mixed variants, one with the delta variant only, two with the alpha and delta variant and only one with the Delta variant. During this discussion, which preceded ACIP’s vote on recommending the Pfizer vaccine, there was no consideration of the effects of the delta variant or of waning immunity described in a post-vote presentation.[22]
Why were data describing waning immunity or effectiveness against delta omitted prior to the vote?
Get out your magnifying glass and look at the small print for slide 6.
Slide 6 from presentation by Dr. Gargano (footnote 15)
“Articles were eligible for inclusion if published before 8/20/21”
This sounds perfectly reasonable except when you look at the evidence presented (footnote 14) in a discussion of booster doses, waning immunity, and the Delta variant that took place AFTER ACIP voted to recommend the Pfizer vaccine.
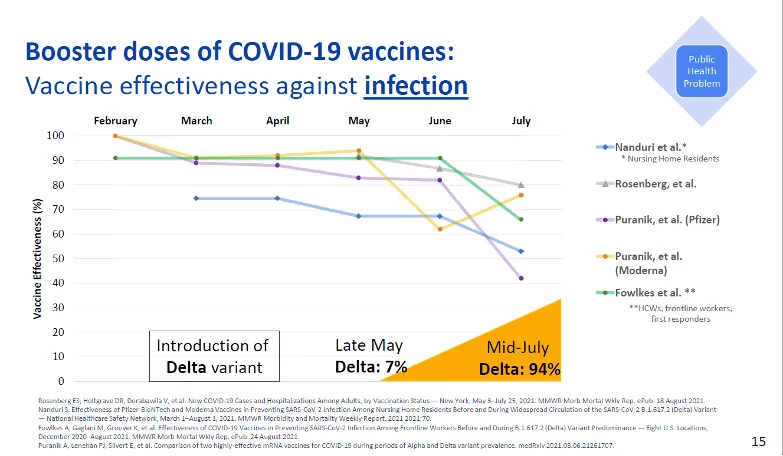
Slide 15 of Dr. Oliver’s presentation shows a waning of vaccine effectiveness to between 40 and 80%.
Slide 15 from presentation of Dr. Oliver (footnote 14)
Why was this waning effectiveness not considered PRIOR to the vote being taken? Surely any recommendation to use the vaccine must take into account prevailing levels of efficacy, regardless of how good it was before? You will answer by saying that CDC needed time to complete their pre-vote analysis, so they had a cutoff date of August 20. Let’s take a look at the four studies shown on this slide.
Nanduri et al. (20) This was a CDC paper showing loss of VE from 74.7% to 53.1% in nursing home residents. The paper was published in CDC’s own journal MMWR (Morbidity and Mortality Weekly Report) on August 27. It was not included in the pre-vote evidence for effectiveness because it did not meet the August 20 cut-off. But we saw earlier how unpublished data (including CDC data) had been incorporated into the pre-vote analysis. There is one more problem here. The Nanduri paper states: “On August 18, 2021, this report was posted as an MMWR Early Release on the MMWR website,” thus meeting the cut-off criteria.
Rosenberg et al., (21) This is another CDC report showing a decline in vaccine effectiveness against infection for New York adults from 91.7% to 79.8%. It was published in MMWR on August 27, with an early release date of August 18.
Puranik et al. (22) This non-peer-reviewed preprint showed a decline to July 2021 in the effectiveness of the Moderna vaccine to 76% and the Pfizer vaccine to 42%. This paper was not authored by CDC staff and was first posted on medrxiv August 8, with revisions posted on August 9 and 21. These revisions showed the same declining effectiveness. This study WAS referenced in the pre-vote presentation by Dr. Gargano (footnote 16), however, the finding of 42% effectiveness against infection does not appear to have been tabulated.
Fowlkes et al. (23) Another CDC paper showed waning immunity from 91% to 66% in front-line workers. This was published in MMWR on August 27, but with an early release date of August 24. Why this was not released on August 18, along with the Nanduri paper is unclear. Another paper by CDC and other authors (24) which showed sustained effectiveness in adults was included in the pre-vote analysis and was published on August 27 in MMWR with an early release date of August 18.
Slide 52 of the same presentation contained a list of 14 references for recent estimates of vaccine effectiveness against the Delta variant, including the four papers cited above.
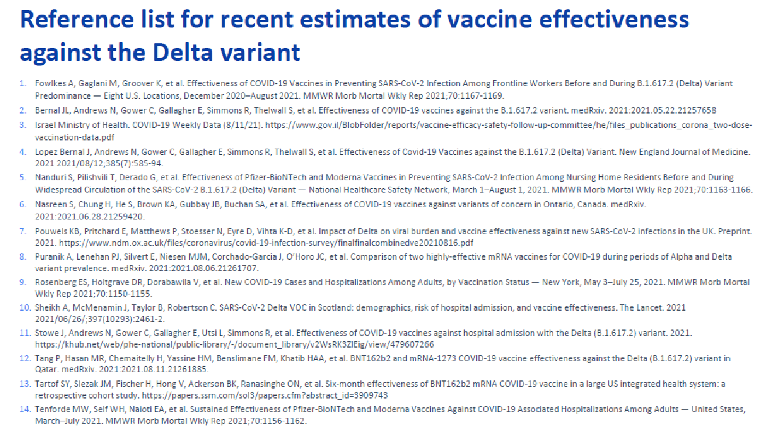
Slide 52 from presentation of Dr. Oliver footnote 14
There were three other papers in this list that also described waning immunity or reduced immunity of the Pfizer vaccine against the Delta variant.
#10. Sheikh et al. (25) The paper itself states that it was published online on June 14, 2021, and stated “Both the Oxford–AstraZeneca and Pfizer–BioNTech COVID-19 vaccines were effective in reducing the risk of SARS-CoV-2 infection and COVID-19 hospitalization in people with the Delta VOC, but these effects on infection appeared to be diminished when compared to those with the Alpha VOC.”
#13. Tartof et al. (26) This study results were:
“For fully vaccinated individuals, effectiveness against SARS-CoV-2 infections was 73% (95%CI: 72‒74) and against COVID-19-related hospitalizations was 90% (89‒92). Effectiveness against infections declined from 88% (86‒89) during the first month after full vaccination to 47% (43‒51) after ≥5 months. Among sequenced infections, VE against Delta was lower compared to VE against other variants (75% [71‒78] vs 91% [88‒92]). VE against Delta infections was high during the first month after full vaccination (93% [85‒97]) but declined to 53% [39‒65] at ≥4 months. VE against hospitalization for Delta for all ages was high overall (93%).”
This preprint was posted on August 23, 2021. It was funded by Pfizer and seven of the 15 authors have their affiliation listed as Pfizer.
The study (#7) by Pouwels et al. (6) WAS included in the pre-vote presentation by Dr. Gargano (footnote 16), despite similar publication dates as the above-mentioned non-included papers. This study examined VE in the Pfizer (BNT162b2), Moderna, and Astra-Zeneca (ChAdOx1) vaccines and concluded: “SARS-CoV-2 vaccination still reduces new infections, but effectiveness and attenuation of peak viral burden are reduced with Delta.”
“Importantly, attenuations in the Delta-dominant period now reached statistical significance for BNT162b2 as well as ChAdOx1 (e.g. Ct<30 VE 14 days post second dose 84% (82-86%) Delta versus 94% (91-96%) Alpha (heterogeneity p<0.0001), and 70% (65-73%) versus 86% (71-93%) respectively for ChAdOx1 (heterogeneity p=0.04)).”
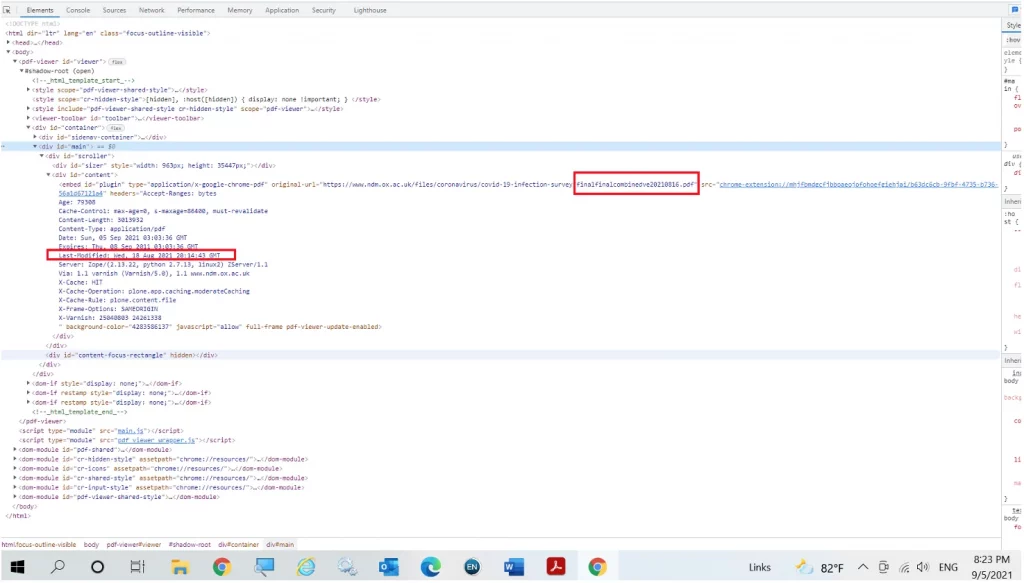
The study was posted as a preprint on medrxiv on August 24. However, as cited by CDC, the study first appeared on the Nuffield Department of Medicine (University of Oxford) website. The file name suggests the date of file to be August 16, 2021. Inspection of the html code for the referenced link reveals the date last modified as Wednesday August 18, 2021.
We see therefore a total of six papers, cited in a presentation AFTER ACIP’s vote, describing waning or reduced immunity against delta appear to have been completely or partially (pertinent part) omitted from the evidence presented (footnote 13) by CDC to ACIP on the benefits and harms of the Pfizer vaccine, PRIOR to its vote on the recommendation. Of these six, four (20-22,25) clearly met the cut-off date for inclusion of August 20. Of these four, one of these (22), WAS referenced in the pre-vote presentation by Dr. Gargano (footnote 16), however, the finding of 42% effectiveness against infection does not appear to have been tabulated.
One study (23) was published as an early release in MMWR on Aug 24, by CDC staff. Another study (26) was posted on August 23 and was funded by Pfizer and included Pfizer scientists. Given the inclusion in the pre-vote CDC presentation (footnote 13) of unpublished data, (footnote 14) despite not meeting the Aug 20 cut-off date, as well as the inclusion of unpublished CDC data in earlier evidence presented (footnote 4) to ACIP, it is difficult to justify why these two studies were omitted from the pre-vote evidence. The apparent omission of a study funded by Pfizer funded (which included as authors Pfizer scientists) (26) from the evidence presented by the Pfizer representative (footnote 12) requires explanation.
Lastly, the August 20 cut-off date for including studies in the evidence (footnote 13) presented immediately before ACIP’s vote appears arbitrary, given their inclusion in the evidence presented after the vote (footnote 15).
How would the inclusion of data showing lower levels of vaccine effectiveness change the risk-benefit analysis?
Once vaccine effectiveness falls from the 90-95% range towards and below 50% any risk-benefit analysis would change greatly, placing these vaccines in close competition with repurposed drugs with far fewer safety concerns, and effectiveness under different scenarios of 30-60% [hydroxychloroquine; (27-29) ivermectin; (30,31) fluvoxamine; (32) Zinc/Vitamin D/other Vitamins (33,34) ]. Options are running out as we race towards authorizing a booster dose. FDA, NIH, and CDC, in appearing to endorse the recent surge in media attacks on repurposed drugs, particularly ivermectin, may have backed themselves into a corner. At the same time, Pfizer has announced that the first patient in their phase 2/3 study received a dose of their proprietary PF-07321332 – a drug intended to treat “non-hospitalized, symptomatic adult participants who have a confirmed diagnosis of SARS-CoV-2 infection and are not at increased risk of progressing to severe illness, which may lead to hospitalization or death.” (35)
If plan A is to rely on the vaccines, and the post hoc plan B to rely on booster doses, is plan C to wait another year for the arrival of PF-07321332?
Booster Doses
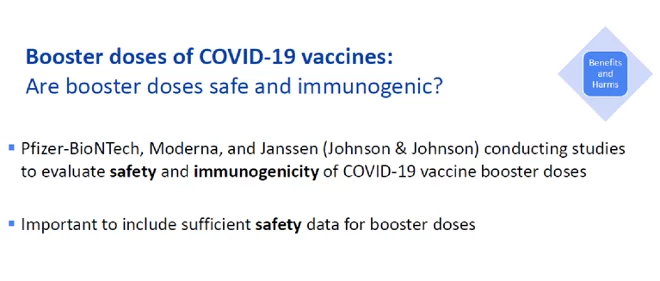
The post-vote discussion on booster doses from Dr. Oliver (footnote 14) focused mainly only on existing data on waning immunity and reduced effectiveness against delta. The discussants recognized the challenges in producing reliable data that could support the use of booster doses and a plan was outlined to be able to obtain data that could support an ACIP recommendation for booster doses following a planned approval by FDA mid- September. It is unclear what data currently exist or would even be available by that time.
Dr. Oliver certainly stated that it was important to determine both the safety and effectiveness of the booster doses.
Slide 29 from presentation of Dr. Oliver (footnote 14)
The use of the term “booster” was questioned and suggested to have less positive connotations than positioning the “third dose” as merely one in a series of a planned course of immunizations, similar to that used for other kinds of vaccines. This has clearly not been the case with the Covid-19 vaccines. Had this been planned, then provision could have been made within the pivotal trials to study the effects of boosters. This is all but precluded now with the substantive loss of blinding in those studies. (36)
Any assessment of safety for third doses must be considered alongside the significant short- and long-term safety questions that remain after two doses.
As for the effectiveness of the third dose, there are few data now emerging. One recent study(37) did suggest that waning or reduced immunity can be restored with a booster dose, but this is only partial, and is at best, according to the study, temporary.
Why was it necessary for ACIP to issue this recommendation?
Extensive discussion preceded the vote based on a presentation: “Evidence to Recommendations Framework: Pfizer-BioNTech COVID-19 vaccine”.[23] One primary concern of that discussion was the issue of vaccine hesitancy. In one survey unvaccinated people were asked:
“Would you be more likely to get vaccinated if one of the vaccines currently authorized for emergency use received full approval from the FDA” (emphasis added)
Of these, “31% of unvaccinated respondents said they would be more likely to get vaccinated after full FDA vaccine approval,” meaning – OF ANY OF THE VACCINES.
This provides the possible rationale for the FDA’s puzzling approval of a vaccine that does not exist. CDC took this to the next step, inferring that not only would FDA approval of ANY of the vaccines be necessary to overcome at least 31% of vaccine hesitancy but that a CDC/ACIP recommendation would also be required.
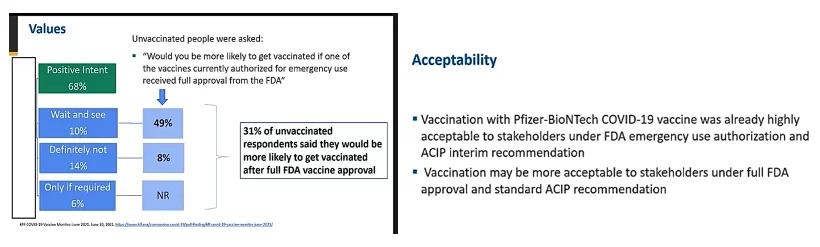
Slides 37 and 43 from presentation by Dr. Dooling (footnote 18)
Accordingly, it was felt that a recommendation from ACIP, such as the one approved, along with full FDA approval (i.e. BLA) for at least one of the vaccines, would be a significant step in reducing vaccine hesitancy. Presumably, this rationale prevailed at FDA when they puzzlingly issued to BioNTech (as opposed to Pfizer/BioNTech) the BLA for a vaccine (COMIRNATY) on August 23 that was not yet available in the USA.
ACIPs recommendation is even more puzzling. Its wording takes no account of the legal reality of there being two legally distinct vaccines as the FDA explains [footnote 8 in (38)]. For this legal distinction to have any meaning, there would need to exist the ability in VAERS to report and track separately the two legally distinct vaccines. We should expect to see under the list of manufacturers both BioNnTech and Pfizer/BioNTech. We do not (9/6/21). The wording of the recommendation is therefore misleading to the point of being meaningless because on the one hand it speaks about the “Pfizer-BioNTech Covid-19 vaccine”(still under EUA) and on the other hand it speaks of BLA approval (COMIRNATY COVID-19 Vaccine, mRNA).
Did scientific misconduct occur?
We pointed out at the outset of this paper, the CDC endorsement of ACIP’s recommendation, once published in MMWRwill “represent the official CDC recommendations for immunizations in the United States.”[24] CDC’s endorsement is already having enormous ramifications as to public policy on vaccine mandates and testing. Accordingly, the evidence presented to ACIP by Pfizer and CDC scientists must meet the highest level of standards for scientific integrity and conduct. The inclusion of key studies evincing lowered effectiveness from the 90-95% range to as low as 42%, would surely have resulted in a different risk-benefit analysis. Is this not akin to the withholding of evidence by lawyers in a trial?
“Scientific misconduct” is defined by CDC [25]
“Under applicable federal regulations found at 42 CFR Part 93 [subpart 103 see [26] (39)], research misconduct is defined as fabrication, falsification or plagiarism in proposing, performing or reviewing research, or in reporting research results. Research misconduct does not include honest errors, differences of opinion, or authorship disputes.” (emphasis added)
I will leave it to the ethicists and lawyers to determine whether or not what happened on August 30 violated any laws, regulations, or codes of ethics. I can only hope that the discrepancies noted in this article are the result of the demands imposed by pandemic conditions that impair the diligence of otherwise well-intentioned people. If that is the explanation, then matters must still be corrected. Uncorrected, for me, none of this passes the smell test. Has Covid has caused everyone to lose their sense of smell.
Sources
1. Wiseman D, Guetzkow, J,, Seligmann H. Comment submitted to August 30 2021 meeting of the Advisory Committee on Immunization Practices (Centers for Disease Control). Docket CDC-2021-0089-0023. 2021 Aug 29. at https://www.regulations.gov/comment/CDC-2021-0089-0023.)
2. Wiseman D. Follow up Comment submitted to August 30 2021 meeting of the Advisory Committee on Immunization Practices (Centers for Disease Control). Docket CDC-2021-0089-0039. 2021 Aug 30. at https://www.regulations.gov/comment/CDC-2021-0089-0039.)
3. Barda N, Dagan N, Ben-Shlomo Y, et al. Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting. N Engl J Med 2021. Epub 2021/08/26 http://doi.org/10.1056/NEJMoa2110475
4. Singer ME, Taub IB, Kaelber DC. Risk of Myocarditis from COVID-19 Infection in People Under Age 20: A Population-Based Analysis. medRxiv 2021:2021.07.23.21260998. Epub Jul 27 http://doi.org/10.1101/2021.07.23.21260998
5. Gupta S, Cantor J, Simon KI, et al. Vaccinations Against COVID-19 May Have Averted Up To 140,000 Deaths In The United States. Health affairs (Project Hope) 2021:101377hlthaff202100619. Epub 2021/08/19 http://doi.org/10.1377/hlthaff.2021.00619
6. Pouwels KB, Pritchard E, Matthews P, et al. Impact of Delta on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. medRxiv 2021:2021.08.18.21262237. Epub Aug 24 http://doi.org/10.1101/2021.08.18.21262237
7. Chau NVVN, Nghiem My; Nguyet, Lam Anh; et al. Transmission of SARS-CoV-2 Delta Variant Among Vaccinated Healthcare Workers, Vietnam. . Alncet Preprints 2021. Epub Aug 10 http://doi.org/http://dx.doi.org/10.2139/ssrn.3897733
8. Kang M, Wei J, Yuan J, et al. Probable Evidence of Fecal Aerosol Transmission of SARS-CoV-2 in a High-Rise Building. Ann Intern Med 2020; 173:974-80. Epub 2020/09/02 http://doi.org/10.7326/M20-0928
9. VAERS. Immunization Safety Office, Division of Healthcare Quality Promotion National Center for Emerging and Zoonotic Infectious Diseases Centers for Disease Control and Prevention. Vaccine Adverse Event Reporting System (VAERS) Standard Operating Procedures for COVID-19. 2021 Jan 29. at https://www.cdc.gov/vaccinesafety/pdf/VAERS-v2-SOP.pdf.)
10. FDA. Package Insert for COMIRNATY. 2021 Aug 23. at https://www.fda.gov/media/151707/download.)
11. Klein NP, Lewis N, Goddard K, et al. Surveillance for Adverse Events After COVID-19 mRNA Vaccination. JAMA 2021. Epub Sep 3 http://doi.org/10.1001/jama.2021.15072
12. FDA. Food and Drug Administration. Long Term Follow-up After Administration of Human Gene Therapy Products. Guidance for Industry. FDA-2018-D-2173. 2020. (Accessed July 13, 2021, at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/long-term-follow-after-administration-human-gene-therapy-products
https://www.fda.gov/media/113768/download.)
13. Moderna. QUARTERLY REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the quarterly period ended June 30, 2020. 2020 Aug 6. (Accessed July 22, 2021, at https://www.sec.gov/Archives/edgar/data/1682852/000168285220000017/mrna-20200630.htm.)
14. FDA. BLA Approval for BioNtech COMIRNATY Vaccine. 2021. (Accessed Aug 23, 2021, at https://www.fda.gov/media/151710/download.)
15. FDA. Summary Basis for Regulatory Action: COMIRNATY. 2021 Aug 23. (Accessed 2021, Aug 25, at https://www.fda.gov/media/151733/download.)
16. Cotton C. VAERS DATA ANALYSIS. 2021 Jul 23. (Accessed Aug 17, 2021, at https://www.francesoir.fr/sites/francesoir/files/fs_vaers_data_analysis_report-2021-08-08.pdf.)
17. Shimabukuro TT, Kim SY, Myers TR, et al. Preliminary Findings of mRNA Covid-19 Vaccine Safety in Pregnant Persons. N Engl J Med 2021; 384:2273-82. Epub 2021/04/22 http://doi.org/10.1056/NEJMoa2104983
18. Zauche LH, Wallace B, Smoots AN, et al. Receipt of mRNA Covid-19 Vaccines and Risk of Spontaneous Abortion. New England Journal of Medicine 2021. Epub Sep 8 http://doi.org/10.1056/NEJMc2113891
19. Thomas SJ, Moreira ED, Kitchin N, et al. Six Month Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine. medRxiv 2021:2021.07.28.21261159. Epub Jul 28 http://doi.org/10.1101/2021.07.28.21261159
20. Nanduri S, Pilishvili T, Derado G, et al. Effectiveness of Pfizer-BioNTech and Moderna Vaccines in Preventing SARS-CoV-2 Infection Among Nursing Home Residents Before and During Widespread Circulation of the SARS-CoV-2 B.1.617.2 (Delta) Variant – National Healthcare Safety Network, March 1-August 1, 2021. MMWR Morb Mortal Wkly Rep 2021; 70:1163-6. Epub 2021/08/27 http://doi.org/10.15585/mmwr.mm7034e3
21. Rosenberg ES, Holtgrave DR, Dorabawila V, et al. New COVID-19 Cases and Hospitalizations Among Adults, by Vaccination Status – New York, May 3-July 25, 2021. MMWR Morb Mortal Wkly Rep 2021; 70:1150-5. Epub 2021/08/27 http://doi.org/10.15585/mmwr.mm7034e1
22. Puranik A, Lenehan PJ, Silvert E, et al. Comparison of two highly-effective mRNA vaccines for COVID-19 during periods of Alpha and Delta variant prevalence. medRxiv 2021. Epub 2021/08/18 http://doi.org/10.1101/2021.08.06.21261707
23. Fowlkes A, Gaglani M, Groover K, et al. Effectiveness of COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Frontline Workers Before and During B.1.617.2 (Delta) Variant Predominance – Eight U.S. Locations, December 2020-August 2021. MMWR Morb Mortal Wkly Rep 2021; 70:1167-9. Epub 2021/08/27 http://doi.org/10.15585/mmwr.mm7034e4
24. Tenforde MW, Self WH, Naioti EA, et al. Sustained Effectiveness of Pfizer-BioNTech and Moderna Vaccines Against COVID-19 Associated Hospitalizations Among Adults – United States, March-July 2021. MMWR Morb Mortal Wkly Rep 2021; 70:1156-62. Epub 2021/08/27 http://doi.org/10.15585/mmwr.mm7034e2
25. Sheikh A, McMenamin J, Taylor B, et al. SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet 2021; 397:2461-2. Epub 2021/06/18 http://doi.org/10.1016/S0140-6736(21)01358-1
26. Tartof SY, Slezak, Jeff M. , Fischer, Heidi, Hong, Vennis, Ackerson, Bradley K., Ranasinghe, Omesh N., Frankland, Timothy B., Ogun, Oluwaseye A., Zamparo, Joann M., Gray, Sharon, Valluri, Srinivas R., Pan, Kaijie, Angulo, Frederick J., Jodar, Luis, McLaughlin, John M., . Six-Month Effectiveness of BNT162B2 mRNA COVID-19 Vaccine in a Large US Integrated Health System: A Retrospective Cohort Study. . SSRN 2021. Epub Aug 23 http://doi.org/dx.doi.org/10.2139/ssrn.3909743
27. Dinesh B, J CS, Kaur CP, et al. Hydroxychloroquine for SARS CoV2 Prophylaxis in Healthcare Workers – A Multicentric Cohort Study Assessing Effectiveness and Safety. J Assoc Physicians India 2021; 69:11-2. Epub 2021/09/03
28. Wiseman D. Missing data and flawed analyses reverse or challenge findings of three key studies cited in Covid-19 Guidelines: Guideline revision warranted for PEP and PrEP use of Hydroxychloroquine (HCQ). Letter to NIH Covid-19 Treatment Guidelines Panel. 2020 31 Dec. at https://osf.io/7trh4/.)
29. Wiseman DM, Kory P, Saidi SA, Mazzucco D. Effective post-exposure prophylaxis of Covid-19 is associated with use of hydroxychloroquine: Prospective re-analysis of a public dataset incorporating novel data. medRxiv 2021:2020.11.29.20235218. Epub July 5 http://doi.org/10.1101/2020.11.29.20235218
30. Wiseman D, Kory, P. Possible clustering and/or drug switching confounding obscures up to 56% reduction of symptom persistence by ivermectin. Data Summary for comment posted to JAMA re: Lopez-Medina et al. OSF Preprints 2021. Epub April 7 http://doi.org/https://doi.org/10.31219/osf.io/bvznd
31. Bryant A, Lawrie TA, Dowswell T, et al. Ivermectin for Prevention and Treatment of COVID-19 Infection: A Systematic Review, Meta-analysis, and Trial Sequential Analysis to Inform Clinical Guidelines. American journal of therapeutics 2021. Epub June 17 http://doi.org/DOI: 10.1097/MJT.0000000000001442
32. Together, Reis G, Silva E, et al. Effect of early treatment with fluvoxamine on risk of emergency care and hospitalization among patients with covid-19: the Together randomized platform clinical trial. medRxiv 2021:2021.08.19.21262323. Epub http://doi.org/10.1101/2021.08.19.21262323
33. Hazan S, Dave S, Gunaratne AW, et al. Effectiveness of Ivermectin-Based Multidrug Therapy in Severe Hypoxic Ambulatory COVID-19 Patients. medRxiv 2021:2021.07.06.21259924. Epub July 7 http://doi.org/10.1101/2021.07.06.21259924
34. Procter MDBC, Aprn FNPCCRMSN, Pa-C MVP, et al. Early Ambulatory Multidrug Therapy Reduces Hospitalization and Death in High-Risk Patients with SARS-CoV-2 (COVID-19). International Journal of Innovative Research in Medical Science 2021; 6:219 – 21. Epub http://doi.org/10.23958/ijirms/vol06-i03/1100
35. Pfizer. First Participant Dosed in Phase 2/3 Study of Oral Antiviral Candidate in Non-Hospitalized Adults with COVID-19 Who Are at Low Risk of Severe Illness. 2021 Sept 1. (Accessed Sep 9, 2021, at https://cdn.pfizer.com/pfizercom/2021-09/First_Participant_Dosed_in_Phase_2_3.pdf.)
36. Doshi P. Covid-19 vaccines: In the rush for regulatory approval, do we need more data? BMJ 2021; 373:n1244. Epub 2021/05/20 http://doi.org/10.1136/bmj.n1244
37. Levine-Tiefenbrun M, Yelin I, Alapi H, et al. Viral loads of Delta-variant SARS-CoV2 breakthrough infections following vaccination and booster with the BNT162b2 vaccine. medRxiv 2021:2021.08.29.21262798. Epub Sep 1 http://doi.org/10.1101/2021.08.29.21262798
38. FDA. Letter to Pfizer – Vaccine Approval. 2021 Aug 23. (Accessed Aug 23, 2021, at https://www.fda.gov/media/150386/download.)
39. Public Health Service Policies on Research Misconduct (Accessed Sept 1, 2021, at ttps://ecfr.federalregister.gov/current/title-42/chapter-I/subchapter-H/part-93.)
Notes
www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/adverse-events.html
[6] www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-08-30/05-COVID-Lee-508.pdf [7] With about 2/3 of the US population vaccinated, we would expect about 5000 per deaths to occur every day from non-Covid-19 causes. Using a conservative 30-day follow up, we would expect to see 150,000 deaths reported in VAERS. As of 8/29/21, 6128 deaths (USA, territories and unknown) have been reported in connection with Covid-19 vaccines (4805 deaths 50 States and Washington DC). The system does not appear to be functioning as designed. [8] This is another safety monitoring system used by CDC in collaboration with Kaiser Permanente. [9] www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-08-30/04-COVID-Klein-508.pdf [10] The get-out-of-jail-free card for these guidance documents is that there are not legally binding. [11] www.nichd.nih.gov/newsroom/news/083021-COVID-19-vaccination-menstruation [12] 9/3/21 – searched under “USA, Territories and Unknown” using the terms AMENORRHOEA, DYSMENORRHOEA, HEAVY MENSTRUAL BLEEDING, HYPOMENORRHOEA, MENORRHAGIA, MENSTRUATION DELAYED, MENSTRUATION IRREGULAR. [13] See www.adhesions.org and www.iscapps.org [14] https://www.fda.gov/drugs/guidance-compliance-regulatory-information/postmarket-requirements-and-commitments [15] www.accessdata.fda.gov/drugsatfda_docs/appletter/2017/761061Orig1s000ltr.pdf [16] www.accessdata.fda.gov/drugsatfda_docs/appletter/2021/761123Orig1s000ltr.pdf [17] www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-08-30/06-COVID-Rosenblum-508.pdf [18] According to one writer, those choosing to remain unvaccinated, rather than being demonized, should be thanked for serving as a valuable control population enabling the effects of vaccines to be more fully evaluated. [19] www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-08-30/02-COVID-perez-508.pdf [20] www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-08-30/07-COVID-Gargano-508.pdf [21] Slide 14 in footnote 13: Polack et al., “additional unpublished data obtained from authors” [22] www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-08-30/09-COVID-Oliver-508.pdf [23] www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-08-30/08-COVID-Dooling-508.pdf [24] www.cdc.gov/vaccines/acip/committee/role-vaccine-recommendations.html [25] www.cdc.gov/os/integrity/researchmisconduct/index.htm [26] https://ori.hhs.gov/FR_Doc_05-9643Featured image is from TrialSiteNews
Appendix: Html code for Pouwels et al paper on NDM Web site August18, 2021 (key sections marked)